
Osseointegration, the process where dental implants fuse with the jawbone, is a crucial step for implant success. It determines their longevity and effectiveness. Understanding osseointegration is key for patients as it allows them to comprehend the journey of their implants, make informed decisions, and set realistic expectations. For dental professionals, a comprehensive understanding of osseointegration aids in precise treatment planning and execution, leading to better patient outcomes. Ultimately, osseointegration is the foundation of successful dental implantology, showcasing the vital interplay between biology and technology in restoring smiles and enhancing oral health.
What is Osseointegration?
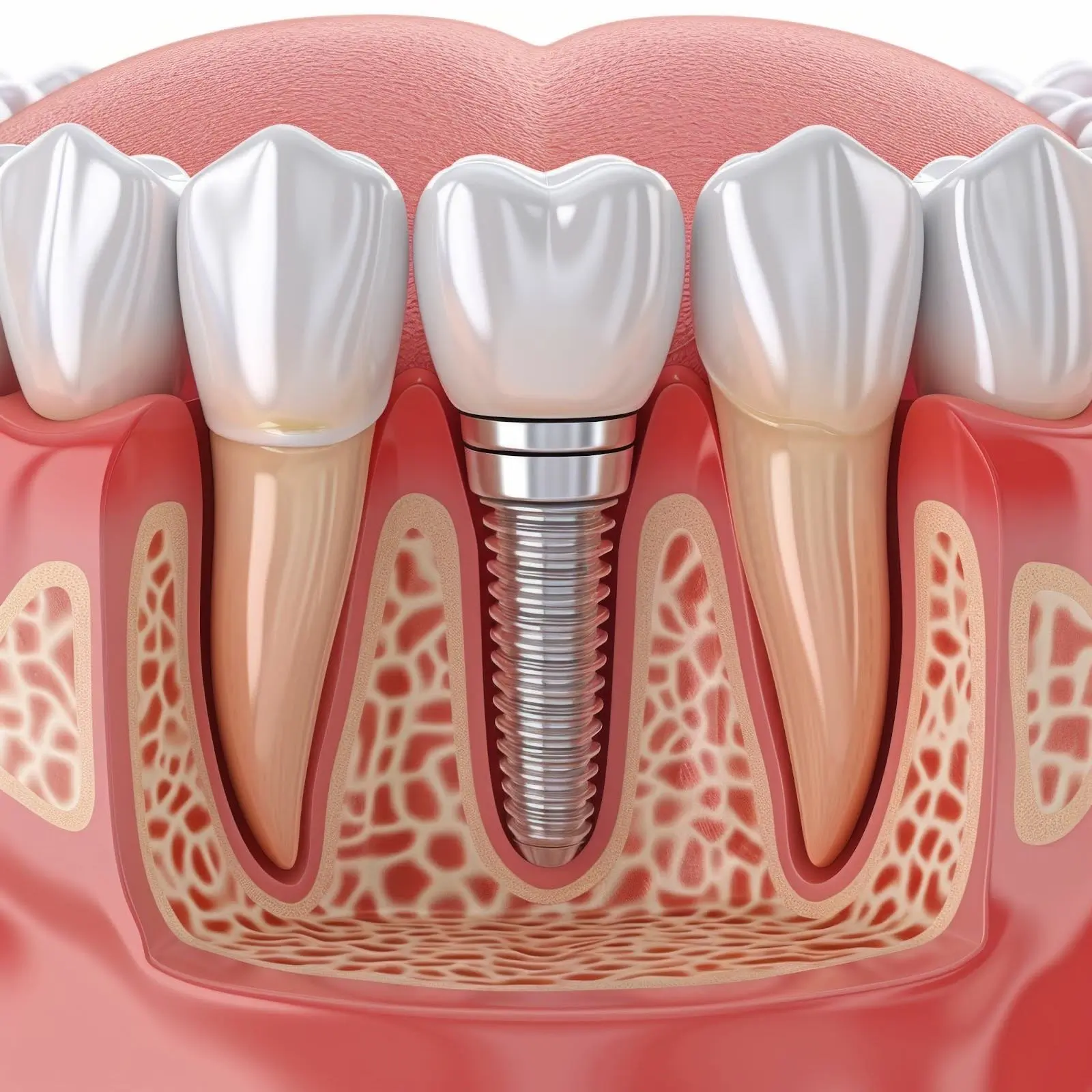
Osseointegration refers to the biological process where dental implants merge with the surrounding bone, creating a stable foundation for prosthetic teeth. Initially, the implant’s surface interacts with bone cells, triggering their adherence and growth. Over time, bone tissue surrounds the implant, anchoring it firmly in place. This intricate bonding mechanism ensures structural support and mimics the natural tooth-root connection, which is essential for the success and functionality of dental implants.
Osseointegration Process
The osseointegration process unfolds in three key phases:
- Initial Healing: This occurs after the implant placement and is when the implant integrates with the surrounding bone surface.
- Bone Formation: The bone cells gradually grow and envelop the implant, fostering structural stability.
- Implant Stability: The bone fully integrates with the implant surface ensuring long-term support.
Several factors influence the speed and success of osseointegration, including implant design, patient bone quality, and post-operative care. Implant design plays a significant role in promoting osseointegration, and understanding its importance can help dental professionals optimize treatment planning and execution, thereby enhancing the durability and efficacy of dental implants.
Role of Implant Design
Implant design plays a pivotal role in facilitating osseointegration by optimizing surface characteristics to enhance bone integration. Modern advancements focus on surface modifications like roughening or adding bioactive coatings to promote faster and more robust osseointegration. Additionally, innovations such as microthreads and tapered designs improve initial stability, accelerating the integration process.
Furthermore, advancements in material science have led to the development of titanium alloys and zirconia implants, offering superior biocompatibility and strength. These cutting-edge technologies underscore the crucial link between implant design and successful osseointegration, driving continuous improvement in dental technology.
Healing and Integration Timeline
Following dental implant placement, osseointegration typically progresses over 3 to 6 months, with bone gradually integrating with the implant surface. However, this timeline can vary depending on the patient’s overall health, bone quality, and implant site location. Conditions such as smoking, diabetes, or insufficient bone density may prolong the process. Conversely, meticulous surgical technique, proper implant selection, and patient compliance with post-operative care can expedite and enhance osseointegration, ensuring optimal implant success.
Factors Affecting Osseointegration
Several factors influence osseointegration, including:
- Bone Quality and Quantity: The density and volume of the jawbone at the implant site significantly influence osseointegration. Dense bone provides better initial stability and facilitates faster integration than softer or less dense bone. Insufficient bone volume may require augmentation techniques such as bone grafting or sinus lifts to create a suitable environment for osseointegration.
- Patient Health: Systemic health factors like diabetes, osteoporosis, autoimmune diseases, and medications can impact bone healing and integration. Diabetic patients, for instance, may experience delayed healing and higher failure rates due to impaired blood circulation and compromised immune response. Smoking is also detrimental to osseointegration as it reduces blood flow and impedes tissue healing.
- Surgical Techniques: Precise surgical planning and execution are critical for successful osseointegration. Factors such as implant site preparation, proper implant placement, and adequate soft tissue management contribute to favorable outcomes. Suboptimal surgical techniques, such as excessive trauma to surrounding tissues or improper implant positioning, can compromise osseointegration and increase the risk of implant failure.
Strategies for optimizing osseointegration include thorough preoperative assessment, augmentation procedures for deficient bone, patient education on lifestyle modifications, and adherence to meticulous surgical protocols. Collaborative efforts between patients, dentists, and specialists are vital for maximizing osseointegration success and long-term implant function.
Osseointegration Success Rates
Osseointegration success rates in dental implant procedures typically range from 90% to 95% over a ten-year period. However, these rates can vary depending on factors like patient health, bone quality, and adherence to post-operative care. Proper patient selection, including thorough medical and dental evaluations and meticulous treatment planning tailored to individual patient needs, is crucial for optimizing osseointegration outcomes.
Importance of Follow-Up Care

Post-operative care during the osseointegration phase typically includes maintaining good oral hygiene, following dietary restrictions, and avoiding habits like smoking. Regular monitoring appointments with the dental provider are essential to assess healing progress, detect any complications early, and ensure optimal osseointegration. These follow-up appointments allow for timely intervention if needed, ultimately contributing to the long-term success of dental implants and patient satisfaction.
Benefits of Successful Osseointegration
Successful osseointegration yields numerous long-term benefits for patients. It ensures enhanced stability and functionality of dental implants, enabling comfortable chewing and speaking. Additionally, implants integrated with the bone provide superior longevity compared to traditional prosthetics, reducing the need for replacements over time. Overall, successful osseointegration contributes to improved oral health, restored aesthetics, and enhanced quality of life for patients with dental implants.
Take the Next Step with Advanced Periodontics & Implant Dentistry!
Your journey to a confident smile begins with expert care and commitment. At Advanced Periodontics & Implant Dentistry, our team is dedicated to ensuring your dental implant journey is seamless and successful. From meticulous surgical techniques to personalized post-operative guidance, we are here every step of the way. Don’t let uncertainties hold you back – call (212) 581-1090 to schedule an appointment today to experience the transformative power of osseointegration and unlock your smile’s full potential!
